The Critical Connection Between Quality CPR and Patient Survival
In the race to save a life during cardiac arrest, the smallest details make the biggest difference. The quality of cardiopulmonary resuscitation (CPR) delivered in those crucial moments determines whether a patient will regain a heartbeat or not.
Definition of ROSC (Return of Spontaneous Circulation)
This vital goal, known as Return of Spontaneous Circulation (ROSC), is the moment when the heart starts beating effectively on its own again, supplying blood to the brain and vital organs.
Statistics on cardiac arrest survival rates
With overall cardiac arrest survival rates still alarmingly low—less than 10% in many communities—the link between high-quality CPR and successful ROSC has never been clearer. Fortunately, advancements in monitoring CPR performance are transforming how healthcare providers approach resuscitation, improving both immediate outcomes and long-term survival.
How Proper Monitoring Transforms CPR Effectiveness
CPR effectiveness hinges on four primary metrics: compression rate, depth, fraction, and recoil. These elements work together to generate adequate blood flow during cardiac arrest. When one metric is off, the entire system falters, reducing the likelihood of ROSC. Monitoring and optimizing these factors in real time is no longer optional—it’s essential for saving lives.
Understanding Key CPR Metrics
Compression Rate
Let’s start with compression rate. The American Heart Association recommends a rate of 100 to 120 compressions per minute for adult patients. This range has been shown to maximize blood flow during CPR. Compress too slowly, and blood fails to reach the organs; too quickly, and the heart doesn’t have time to refill between compressions. Unfortunately, rescuers often veer outside this optimal range, especially under stress. That’s why real-time tools such as metronomes and CPR feedback devices are crucial for maintaining consistency and improving patient outcomes.
Compression Depth
Next is compression depth. High-quality compressions must reach a depth of at least two inches (5 cm) in adults to create enough pressure to circulate blood. Shallow compressions simply don’t push blood where it needs to go. However, going too deep can cause rib fractures or internal injuries, particularly in elderly patients. Achieving the right depth consistently requires good technique and continuous monitoring—something that’s difficult without real-time feedback.
Compression Fraction
Compression fraction refers to the percentage of time during a resuscitation attempt that compressions are actively being delivered. Experts recommend a target of at least 80%. This means that for every minute of CPR, compressions should be ongoing for at least 48 seconds. Interruptions—whether for pulse checks, airway placement, or rhythm analysis—must be minimized. The longer the hands-off time, the lower the chance of ROSC. Monitoring devices that track compression fraction help teams identify and reduce unnecessary pauses.
Chest Recoil
Then there’s chest recoil. After each compression, the chest must fully return to its natural position to allow the heart to refill with blood. Incomplete recoil reduces venous return, which in turn decreases the effectiveness of the next compression. Leaning on the chest or compressing too quickly without allowing full release can severely limit circulation. Real-time feedback helps ensure proper recoil is maintained with each cycle.
Real-Time Monitoring Technologies
Technology is playing a key role in tracking these vital metrics. CPR feedback devices—many of which use accelerometers or force sensors—give audio and visual cues during resuscitation. Some are integrated directly into the defibrillator, offering immediate coaching on compression quality and rhythm analysis. These tools not only help during active resuscitation but also provide valuable data for post-event review.
Defibrillators with built-in CPR coaching capabilities further enhance performance. These systems can display waveform analysis, guide providers with prompts, and store data for later review. This combination of real-time and retrospective feedback allows teams to refine their techniques and identify areas for improvement after each event.
Mobile apps are also making an impact. From metronomes that help rescuers maintain proper compression rates to training apps with built-in feedback mechanisms, digital tools are bringing CPR quality control into everyday practice. Many also include documentation and tracking features that simplify post-resuscitation reporting and data analysis.
The Science Behind ROSC Improvement
Coronary Perfusion Pressure & Cerebral Blood Flow
The physiological basis for all of this technology centers on maintaining coronary perfusion pressure—the force that pushes blood into the coronary arteries. Studies show that high-quality chest compressions are the only way to generate enough pressure to keep the heart viable during arrest. Similarly, proper CPR technique supports cerebral blood flow, which is essential for preserving brain function and preventing long-term neurological damage.
Research Evidence
Research continues to confirm that high-quality CPR—measured and optimized in real time—significantly increases ROSC rates. Feedback devices and structured training programs are consistently associated with improved outcomes in both in-hospital and out-of-hospital cardiac arrests. Moreover, survival to discharge and favorable neurological outcomes are also higher when CPR metrics are closely monitored and adjusted during the event.
Implementing CPR Quality Programs
Implementing CPR quality monitoring in healthcare settings involves more than purchasing new tools. Institutions must develop protocols that prioritize metric tracking during code. This includes training staff to use devices correctly, assigning roles during emergencies, and integrating quality assurance into daily practice.
Team-Based Approaches
A team-based approach enhances effectiveness. Clear communication protocols, assigned roles, and regular debriefings after resuscitation events help teams identify what worked and what didn’t. Over time, this fosters a culture of continuous improvement, where every code becomes a learning opportunity.
Documentation and Analysis
Documentation plays a critical role as well. Recording CPR metrics during and after events allows healthcare organizations to identify trends, address gaps in training, and measure the effectiveness of interventions. This data can inform future training sessions and drive performance improvement efforts.
Training and Skill Development
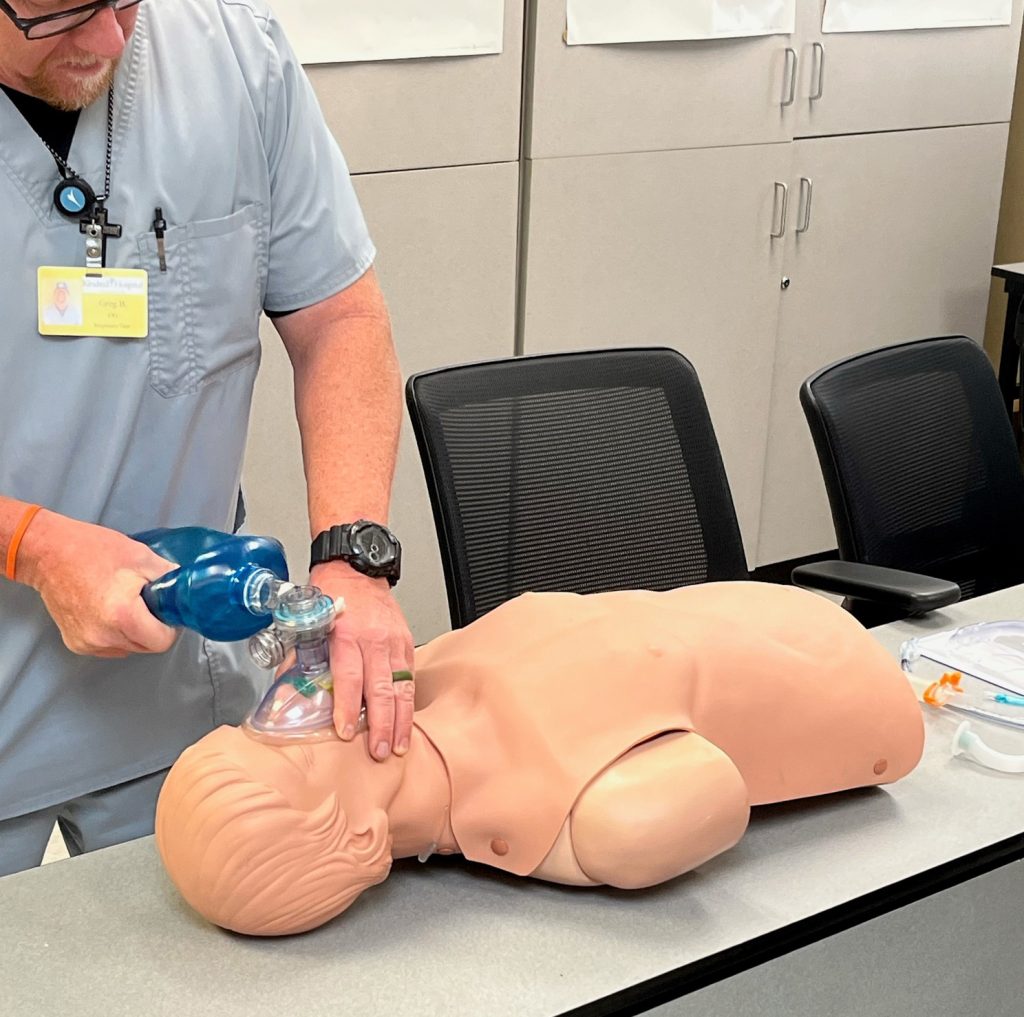
Speaking of training, building these skills starts with simulation-based learning. High-fidelity mannequins provide real-time feedback on compression rate, depth, and recoil, allowing students to practice in realistic scenarios. Immediate correction helps embed proper technique and muscle memory.
Competency Assessment
Competency assessments ensure providers meet baseline standards. These evaluations, paired with ongoing education and recertification, help combat skills decay. Refresher training—ideally every six months—reinforces critical knowledge and adapts to evolving guidelines.
Overcoming Common Challenges
Stress and Performance
Of course, challenges exist. Stress during actual resuscitations can cause even seasoned providers to forget technique or overlook key metrics. Training under pressure helps condition responders to maintain quality even in chaotic settings. When feedback devices are unavailable, manual techniques such as counting aloud or using a metronome can be helpful.
Equipment Limitations
Equipment limitations also occur. Teams should have backup plans for when technology fails, such as assigning someone to count compressions or monitor timing manually. Coordination among rescuers remains essential, especially during handoffs or when switching roles.
Conclusion
Ultimately, improving ROSC rates depends on a combination of science, technology, training, and teamwork. Monitoring CPR metrics isn’t just a best practice—it’s a life-saving strategy. As more healthcare providers embrace data-driven resuscitation, survival rates and neurological outcomes will continue to improve.
Take the next step in your professional development. Contact CPR Tampa today to schedule your American Heart Association-certified training. Our stress-free, hands-on approach ensures you’ll gain confidence in CPR monitoring techniques that truly save lives. Visit https://acls-bls-tampa.com/ or call 727-240-9404 to enroll in BLS, ACLS, PALS, or CPR and First Aid courses.


