When a person suddenly collapses and stops breathing, the immediate commencement of cardiopulmonary resuscitation, or CPR, is a critical step that can bridge the gap between sudden death and survival. The basic principles of CPR involve delivering high-quality chest compressions and rescue breaths to maintain circulation and provide oxygen until definitive care arrives. While the rhythmic press of chest compressions keeps blood moving, maintaining an open airway and ensuring effective ventilation is equally vital, forming the foundational core of resuscitation. For the professional rescuer working in an emergency medical service, hospital, or other advanced life support setting, the standard rescue breath techniques evolve into something far more sophisticated and effective: the implementation of an advanced airway. This advanced airway in CPR moves beyond basic techniques, dramatically changing the way providers manage a patient’s breathing during cardiac arrest. The purpose here is to clearly define what qualifies as an advanced airway, explain the key differences it introduces to the CPR process, and emphasize why every healthcare professional needs proper advanced airway management training.
What is Considered an Advanced Airway?
Defining an advanced airway in CPR distinguishes professional-level life support from bystander or basic life support. Simply put, an advanced airway is a device placed into the patient’s trachea, or windpipe, that creates a secure, sealed conduit directly into the lungs. This bypasses the upper airway, stomach, and esophagus, offering a superior method for oxygen delivery and ventilation. These sophisticated airway devices fall into several categories. The most definitive example is the endotracheal tube, or ET tube, which requires specialized training for correct placement through the vocal cords. Another increasingly common category involves supraglottic airway devices, which sit above the glottis to seal the entrance to the larynx. Examples include the Laryngeal Mask Airway, or LMA, the i-gel, and the King airway. It is crucial to clarify that these advanced airway devices are reserved exclusively for use by highly trained healthcare providers, such as paramedics, respiratory therapists, nurses, and physicians, and they are not intended for use by lay rescuers. The American Heart Association, or AHA, guidelines incorporate the use of these devices into their Advanced Cardiac Life Support, or ACLS, protocols, guiding providers on their proper selection and placement during resuscitation efforts.
The most significant change an advanced airway in CPR introduces is the complete restructuring of the compression-to-breath ratio, altering the flow of resuscitation. In standard basic life support, or BLS, where no advanced airway is in place, rescuers use a 30:2 ratio, pausing chest compressions after every thirty compressions to deliver two rescue breaths. This interruption, though brief, temporarily halts blood flow. With an advanced airway, however, this crucial difference disappears. Instead of interruptions, the team performs continuous chest compressions. Simultaneously, the designated rescuer delivers asynchronous breaths. This means the chest compressions never stop for ventilation, which significantly minimizes “hands-off time” and maximizes blood flow to the brain and vital organs. The presence of a sealed airway, like an endotracheal tube, provides immense benefit by maintaining a secure, open passage and reducing the risk of interruptions in chest compressions. Furthermore, a correctly placed advanced airway helps ensure improved oxygenation and simultaneously reduces the risk of aspiration, preventing stomach contents from entering the lungs, a frequent complication in unsecured airways.
Basic vs. Advanced Airways: Key Differences
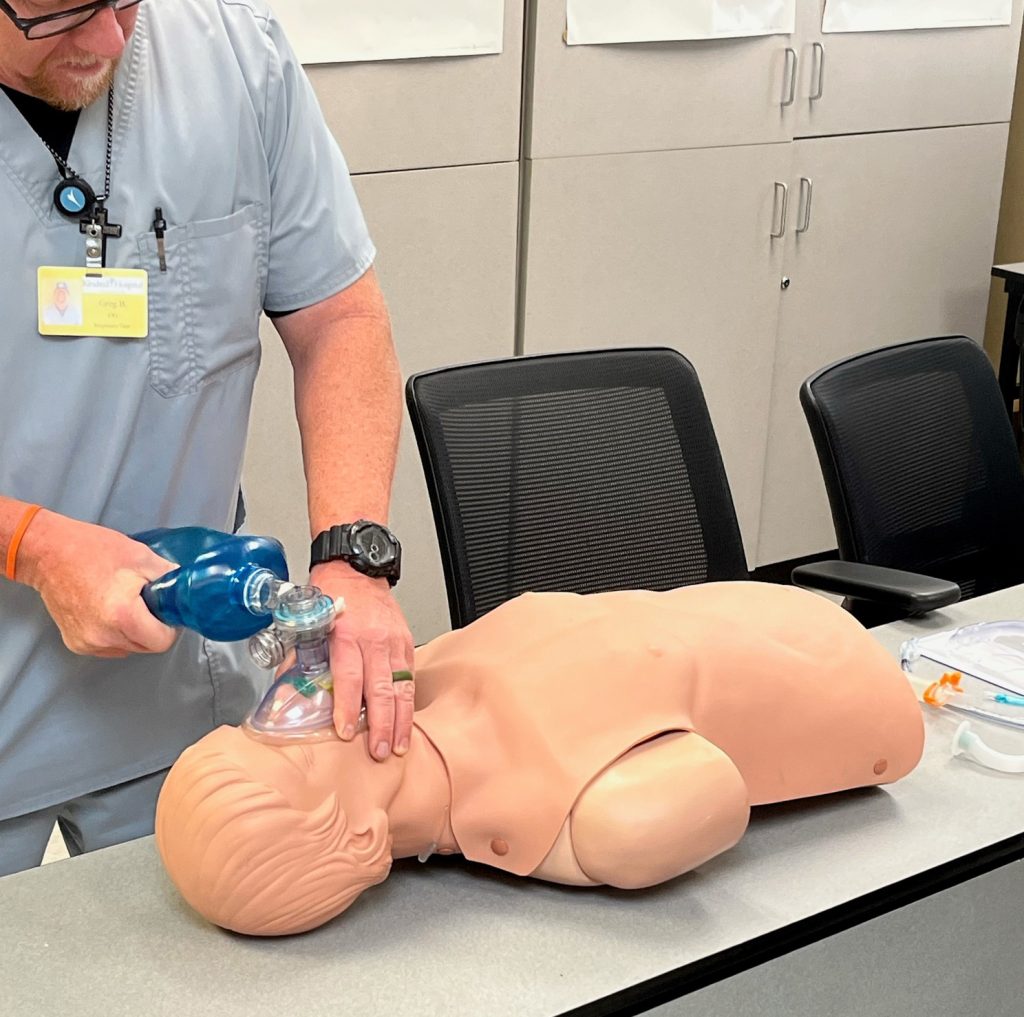
To fully appreciate the role of advanced airway management, one must first recognize the differences between basic and advanced techniques. Basic airway management techniques are simple, non-invasive maneuvers that anyone can perform, such as the head tilt-chin lift or jaw thrust. They also include the use of simple tools like the bag-mask ventilation, or BVM, device, or the insertion of oropharyngeal or nasopharyngeal airways to temporarily move the tongue and soft tissue out of the way. Advanced airway management, by contrast, involves invasive procedures that physically secure the airway. This primarily includes endotracheal intubation and the insertion of supraglottic devices. In extremely rare emergency circumstances when these conventional methods fail, a provider might have to perform a surgical airway, such as a cricothyrotomy. The following comparison clearly illustrates why specialized training is essential:
- Basic Airway Management: Requires minimal skill, uses a BVM or simple plastic devices, is used by all rescuers, and offers temporary assistance with a high risk of gastric inflation.
- Advanced Airway Management: Requires extensive skill and training, uses advanced airway devices like the ET tube, used only by trained healthcare providers, and offers a secure, sealed airway with reduced aspiration risk.
What is the Breath Rate for Advanced Airway CPR?
Moving to the specifics of ventilation, understanding the correct breath rate for advanced airway CPR is fundamental to effective resuscitation. The tendency for many novice rescuers is to breathe too fast, a phenomenon known as hyperventilation, which can be detrimental to patient outcomes. Excessive positive pressure ventilation can actually increase pressure within the chest cavity, which paradoxically reduces the amount of blood that returns to the heart and lowers the effectiveness of chest compressions. To counteract this, the AHA provides a clear, evidence-based recommendation. When an advanced airway is in place, rescuers should deliver one breath every six seconds, which equates to ten breaths per minute, while continuous chest compressions are being performed. Adherence to this slow, deliberate breath rate is a key marker of professional-level care and is a crucial metric monitored during real-world performance assessments. Tying this practice back to provider training helps ensure that the theoretical knowledge translates into life-saving action, emphasizing the importance of precise, unhurried ventilation.
Why Understanding Advanced Airway in CPR Matters
Ultimately, understanding the proper use of an advanced airway in CPR matters because it directly impacts patient survival rates. These techniques are not just academic concepts; they are the tools that separate routine emergency care from advanced life support. Whether in the chaotic environment of an accident scene managed by Emergency Medical Services, a patient’s bedside in a hospital critical care unit, or a cardiac arrest scenario in an advanced life support setting, the rapid and correct deployment of an endotracheal tube or supraglottic airway device provides the highest quality of oxygenation possible.
FAQs
When should an advanced airway be used during CPR?
An advanced airway should be considered when basic airway techniques like head-tilt-chin-lift and bag-mask ventilation are inadequate or unsuccessful. Healthcare providers typically insert an advanced airway when a patient cannot maintain their own airway, requires prolonged ventilation support, or when effective bag-mask ventilation cannot be achieved. During cardiac arrest, the decision to place an advanced airway depends on the provider’s skill level, the clinical situation, and whether it can be done without prolonged interruptions to chest compressions.
What’s the difference between basic and advanced airway management in CPR?
Basic airway management uses simple techniques like head positioning, jaw thrust maneuvers, and bag-mask ventilation to maintain an open airway. Advanced airway management involves inserting a device directly into the airway, such as an endotracheal tube or supraglottic airway device. Advanced airways provide a more secure airway, reduce the risk of aspiration, and allow for continuous chest compressions without pausing for ventilations. However, they require specialized training and carry risks if inserted improperly.
Can I learn about advanced airways in a BLS certification course?
BLS (Basic Life Support) courses focus on fundamental CPR skills, including basic airway management techniques like bag-mask ventilation. Advanced airway insertion and management are typically covered in ACLS (Advanced Cardiovascular Life Support) courses, which are designed for healthcare professionals who may need to manage critical cardiac emergencies. If you’re interested in learning advanced airway techniques, enrolling in ACLS training after completing your BLS certification is the appropriate next step.
How do chest compressions change once an advanced airway is in place?
Once an advanced airway is properly placed and secured, the CPR approach shifts from cycles of compressions and ventilations to continuous compressions with asynchronous ventilations. Rescuers provide chest compressions continuously at a rate of 100-120 per minute without pausing, while another provider delivers one breath every 6 seconds (10 breaths per minute). This method maximizes perfusion during cardiac arrest and improves outcomes by minimizing interruptions to blood flow.
Call to Action
Ready to master life-saving skills? CPR Tampa, an American Heart Association training site, offers comprehensive CPR certification in Tampa and BLS classes in Tampa that prepare you for real-world emergencies. Whether you need initial certification or renewal in BLS for Healthcare Providers, ACLS, PALS, or CPR and First Aid, our stress-free, hands-on courses give you the confidence to respond effectively. Don’t wait—enroll today at best CPR classes in Tampa and become certified to save lives!